Table of Contents
Eczema is a common skin condition that affects millions of people. Is eczema an autoimmune disease? It is not precisely the problem. Still, we’ll examine eczema’s potential connections to autoimmune dynamics.
Additionally, we’ll explore the relationship between autoimmune disorders and other conditions. Get ready to unravel the puzzle of autoimmune versus immunodeficiency.
Eczema and autoimmune disease: Is there a link?
Eczema includes immunity-related problems such as inflammation and allergy-like conditions. But is there a link between eczema and the complexities of autoimmune diseases?
Eczema: The skin dilemma
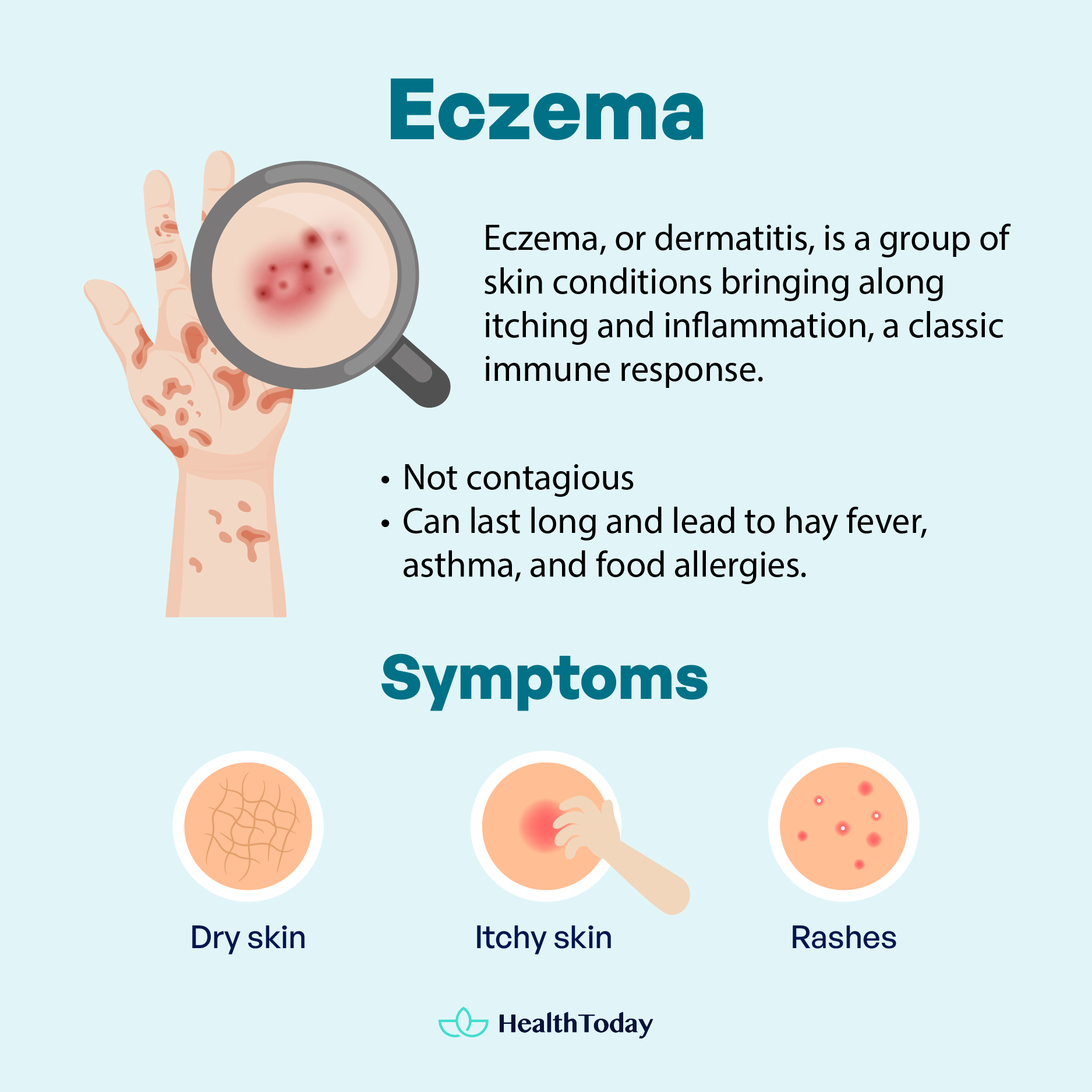
Eczema is a broad term for itchy and inflamed skin conditions. It is also called dermatitis, where ‘itis’ means ‘inflammation’ (1, 2).
The exact cause of eczema remains a mystery, but it can be influenced by genetics and environmental factors. One theory is that eczema occurs due to skin dysfunction, but that’s more likely the result than the reason (3, 4).
Eczema often leads to dry, itchy skin and rashes on the face, inside elbows, behind knees, hands, and feet (1).
Eczema is not contagious or can’t be spread. It can last long, sometimes in combination with hay fever, asthma, and food allergies (1, 3).
Autoimmune diseases: Battling from within
A strong immune system protects your body from sickness, infections, toxins, and cancers by making antibodies to eliminate harmful substances (5, 6).
However, if the immune system malfunctions, it can’t distinguish between healthy tissue and threats. Thus, it may mistakenly attack our body’s organs, tissues, and cells. It is called an autoimmune disease, which can be life-threatening (5, 7).
In America, over 24 million people have autoimmune diseases (7), which come in more than 90 different types (5, 8, 9). The exact cause is uncertain, but genetics may play a role (5, 6).
Common autoimmune diseases include (5, 10, 11, 12):
- Alopecia areata—attacks hair follicles
- Celiac disease—damages the small intestine
- Inflammatory bowel disease (IBD)—mainly includes Crohn’s disease and ulcerative colitis
- Dermatomyositis—causes muscle weakness
- Reactive arthritis—involves joint inflammation
- Rheumatoid arthritis—triggers joint pain and swelling
- Sjögren syndrome—attacks glands that produce moisture
- Systemic lupus erythematosus—hampers different body parts
- Type I diabetes—targets the pancreas cells
- Vitiligo—destroys melanocytes (cells for skin pigment)
Skin is one of the areas that are commonly impacted by autoimmune diseases (5).
The possible connection
Both eczema and autoimmune disease involve inflammation caused by immune cells and proteins, suggesting a potential common mechanism (4, 5).
Research suggests that having eczema or a family history of it may increase the risk of autoimmune problems (9, 13).
Atopic dermatitis (AD) is the most common type of eczema (1). A large population-based study found that people with AD have a 97 percent higher risk of developing autoimmune diseases, particularly those affecting the skin, gut, or connective tissue (13).
Similar studies show that people having an autoimmune disease are more prone to other autoimmune disorders (9, 14). The same goes for people with AD, who are more likely to have (9, 13):
- Alopecia areata
- Celiac disease
- Crohn’s disease
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Ulcerative colitis
- Vitiligo
Eczema, or dermatitis, is a group of skin conditions causing itching and inflammation, a classic immune response. Autoimmune responses occur when the immune system attacks the body. Eczema and autoimmune disease are connected, as people with eczema are more prone to autoimmune disorders.

Is atopic dermatitis an autoimmune disease?
Atopic dermatitis (AD), or topic eczema, is a common skin disease causing intense itching, dryness, redness, and irritation. Another common sign is rashes that may ooze clear fluid or bleed when scratched (2, 15, 16).
AD affects at least 230 million people worldwide, with most cases occurring before a child reaches the age of one (2, 9). Researchers have found a strong connection between atopic dermatitis and autoimmune diseases.
Understanding atopic dermatitis
The term “atopic” suggests a link to allergies, but it’s not always the case (2). Up to 60 percent of AD patients will later develop asthma or hay fever (allergic rhinitis), and up to 30 percent will have food allergies (2).
Allergens from outside environments can trigger inflammation in about one-third of AD cases (8). However, some experience inflammation even without allergens, suggesting that AD symptoms can also originate internally (8).
Atopic dermatitis has no single cause, but it is commonly agreed that the skin can be damaged when it loses moisture (8, 16). Experts suggest that a combination of genetic factors, environmental influences, and a sensitive immune system can alter the skin’s moisture barrier. Some evidence suggests that autoimmunity could be involved (8).
In the early stage, the skin may be red, swollen, blisters, or weeping. In the later stage, the skin becomes thick and rough (15, 16).
Can it be an autoimmune disease?
Experts suggest dermatitis happens when the immune system overreacts (8). Studies also revealed that interleukins (immune proteins) can be involved (4).
Monoclonal antibody therapies, such as the drug dupilumab, can treat AD by blocking immune proteins while enhancing skin barrier and regulating genes (17, 18, 19, 20).
Dupilumab inhibits two interleukins, IL-4 and IL-13, which normally bind to cells, causing them to produce immune cells that help the body fight viruses and bacteria. By blocking IL-4 and IL3 from binding, it prevents the body from overproducing immune cells which may be associated with atopic dermatitis. Sometimes, these immune cells mistakenly attack healthy tissues, causing an autoimmune reaction (17, 21).
However, it does not necessarily mean eczema is an autoimmune disease.
In addition, eczema patients can have breaks in their skin due to inflammation, making them more likely to get infections from viruses, fungi, or bacteria like Staphylococcus (22, 23, 24). About 60 to 90 percent of AD patients are likely to have staphylococcus bacteria on their skin, which could lead to infection if their skin has open wounds (25). If this occurs, persons with Atopic Dermatitis can have immune cells that overact, which could contribute to the severity of atopic dermatitis (3, 20, 21).
The answer to “Is dermatitis an autoimmune disease?” is “not really.” More research is needed to confirm the term.
Dyshidrotic eczema and autoimmune disease – Plus other types
Dyshidrotic, or pompholyx, eczema is a common type that causes itchy small blisters on the hands and feet, causing scaly skin patches (26). The word “Pompholyx” comes from the Greek word for “bubble” (26).
The cause of this condition is unknown. It usually happens during specific times of the year. It goes away on its own, but sometimes it can become chronic (26, 27).
You may develop pompholyx eczema if you (26, 28):
- are stressed
- have allergies, like hay fever
- live in a hot climate
- have dermatitis elsewhere on your body
- often have wet or damp hands
- work with materials containing chromium, cobalt, or nickel
Not many studies have investigated how the immune system responds in people with dyshidrotic eczema. Thus, it is unclear whether it has an autoimmune factor.
Atopic dermatitis (AD) is not an autoimmune disease, but it shares some inflammatory pathways. Patients with AD may have overactive or dysfunctional immune responses, but it’s unclear whether external infections or internal immunity are the root cause. Scientists may not classify dyshidrotic eczema as an autoimmune disease.





Best ways to prevent eczema and its flare-ups


Entirely preventing eczema can be difficult, especially if it’s genetic. However, you can take some steps to reduce the risk (1, 3, 16, 29, 30):
- Managing allergies: Consult with your doctor or allergist to manage irritants like foods, pet dander, rough fabrics, lotions, or scented products.
- Identifying your triggers: Some triggers can worsen your eczema, such as pollen, wool, strong soaps or harsh detergents, dyes, and lanolin. Also, be careful with air pollutants and tobacco smoke.
If you have eczema or its symptoms, see a dermatologist for a precise diagnosis and personalized advice. The best eczema treatment is keeping your skin moisturized (31). You can use a fragrance-free ointment like petroleum jelly two or three times a day. Ointments are better than creams since they have more oil than water (3, 31).
Ensure your moisturizer doesn’t have preservatives, alcohol, scents, dyes, or other chemicals. Using a humidifier at home can also be beneficial (29, 30).
When you wash or bathe, try to limit the scrubbing and the time in the water, as it can remove natural skin oils. Use a gentle body wash instead of regular soap, and opt for lukewarm baths over hot ones (29, 31).
After bathing, apply moisturizing ointment to lock in moisture and preserve a healthy skin barrier (29). You can also manage the flare-ups and more severe conditions by (22, 29, 30):
- Keep your nails short to prevent scratching.
- Avoid sudden temperature changes. Sudden heat waves, dry air, and sweat can dry out your skin.
- Wear comfy, soft clothes that let your skin breathe. Also, control your room temperature and humidity.
- Improve your sleep. Talk to your doctor if itching disrupts your sleep.
- Manage your stress. Stress can worsen eczema symptoms. Try deep breathing, meditation, yoga, or mindfulness.
- Seek counseling if stress-reduction methods don’t help. Consult with a mental health professional or your loved ones for some advice.
- Skip the smallpox vaccine. Atopic dermatitis may increase your risk of serious complications to the smallpox vaccine. Avoid contact with recently vaccinated people (32).
Preventing eczema and its flare-ups







Autoimmune vs. immunodeficiency disorders
As you age, your immune system becomes less effective (33).
Autoimmune disorders encompass overactive immune responses mistakenly against the body’s healthy tissues (6), as the immune system can’t distinguish self and non-self elements (5, 7). This can lead to chronic inflammation, changes in organ function, and abnormal organ growth (5).
Symptoms vary depending on the type and location of the immune response. Common symptoms include fatigue, fever, malaise, joint pain, and rashes (5).
Immunodeficiency disorders refer to a weakened or impaired immune system, making it struggle to fight infections effectively (33, 34).
You may have an immunodeficiency disorder if you get frequent or persistent infections, experience severe infections from typically harmless germs, or take a long time to recover from illnesses (33). Autoimmunity and immunodeficiency are separate conditions, but they can be related in complex ways. In rare cases, a gene defect can lead to a disease with both autoimmune and immunodeficiency symptoms. Some genetic mutations causing immunodeficiency are also linked to rheumatic (a type of autoimmune) diseases (35).





What autoimmune disease is associated with eczema?
If you have eczema, your risk of developing an autoimmune disease, especially those affecting the skin, gut, or connective tissue, is significantly higher (13).
These associated autoimmune diseases include alopecia areata (hair loss), inflammatory bowel disease (IBD), celiac disease, vitiligo (skin depigmentation), rheumatoid arthritis (joint pain), and lupus (2, 9).
Do people with eczema have a weak immune system?
Which vitamin fights eczema?
While no specific vitamin cures eczema, certain vitamins can support skin health and the immune system, potentially helping manage symptoms.
In some studies, people who took vitamin supplements, including Vitamin D3 and B12, had less severe eczema than people who did not. Vitamin E and vitamin C may also be helpful by reducing inflammation and boosting your skin barrier (4).
Is eczema related to gut health?
Gut health is linked to immune and skin health. Thus, an imbalance in the gut microbiome can contribute to skin problems, including eczema (37). Eczema patients often have a less diverse gut microbiome with more harmful substances and fewer anti-inflammatory compounds (30, 37).
In addition, patients with inflammatory bowel diseases (IBD) can suffer from essential fatty acid deficiency due to malabsorption, which can make their skin dry and more likely to have eczema (10).
What triggers an eczema flare-up?
Eczema flare-ups are often triggered by allergens and irritants like rough materials, fragrances, pollen, dust mites, mold, and certain foods (3, 29). Scratching the skin can also make it worse, which produces more redness, swelling, and itching (1, 2). Hormonal changes during the menstrual cycle can worsen the condition (19).
What diseases have eczema as a symptom?
While eczema can occur as a standalone condition, it can also be a sign of other health issues. It is associated with food allergies and contact with allergens (29). Persons with irritable bowel syndrome (IBS) can also develop skin conditions, including eczema, due to not getting enough vitamins (10).
Moreover, while not a classic symptom, eczema might be more prevalent in people with autoimmune diseases and immunodeficiency disorders (2, 9). Yet, it is unclear if eczema is a cause or symptom of these conditions.
Summary
Eczema is a group of skin conditions that cause inflammation and itching.
Is eczema an autoimmune disease? Eczema doesn’t attack our own cells or organs, so the answer is no.
Scientists have not found a direct link between dyshidrotic eczema and autoimmune diseases. Yet, there is a possible connection between autoimmune disorders and atopic dermatitis (AD).
It is more important to focus on caring for eczema than to classify it. Keep your skin moisturized and use steroid creams for flare-ups.

















Comments
0