Table of Contents
Imagine you’re 25 years old and have had low back pain for a few years. Your doctors haven’t been too concerned about it until you begin experiencing pain in your hips and bowels. You even start to have some blurry vision and constantly feel fatigued. After seeing more doctors and getting tests done, you finally receive a diagnosis of spondyloarthritis (SpA) from a rheumatologist.
How did it take so long to figure this out? SpA is challenging to detect because no single test or symptom provides a definitive diagnosis. Given how difficult it is to identify SpA, paying close attention to all signs and symptoms is crucial.
In fact, hip and gastrointestinal (bowel) pain can be important clues. Hip involvement has been reported in up to 36 percent of patients with one form of SpA called axial spondyloarthritis (ax-SpA). While symptoms of irritable bowel syndrome, including gastrointestinal pain, may occur in 25 percent of people with ax-SpA (1, 2).
Read on to further explore how pain in the hips and gastrointestinal tract can be related to SpA.
What is spondyloarthritis?
Spondyloarthritis is a mouthful, but dissecting the word can help us understand it more easily. The ending “-itis” means inflammation. “Spondylo-” means related to the spine, and “arthritis” refers to inflammation of the joints. Putting it all together, “spondyloarthritis” means inflammation of the spine and joints.
Doctors use the term “axial SpA” to describe SpA that primarily involves the spine, and “peripheral SpA” when the joints outside of the spine (such as the shoulders, elbows, fingers, knees, or ankles) are mostly involved.
However, some people can have features of both axial and peripheral SpA. Other types include ankylosing spondyloarthritis, enteropathic spondyloarthritis, reactive arthritis, and psoriatic arthritis.
A recent review, which included 64 studies across various countries, found that it takes an average of 6.7 years from the symptom onset to a diagnosis of ax-SpA (3). In a study conducted in the United Kingdom, 14 percent of people with symptoms of ax-SpA saw their general practitioner more than ten times before receiving a diagnosis (4).
Signs and symptoms

The main symptom of SpA is pain in the back and joints. Many people who have chronic back or joint pain do not have SpA. Thus, it is not always easy to determine whether these symptoms are related to SpA. However, some clues about the pain can point to SpA, including (5):
- Low back pain that lasts more than three months (ax-SpA)
- Pain that begins in young adulthood, typically in the 20s and 30s
- Morning stiffness that lasts longer than one hour
- Stiffness that improves with activity and worsens with rest
- Pain that is worse on one side of the body compared to the other
- Pain in the heel due to Achilles tendonitis (peripheral-SpA)
- Swelling in the fingers and toes (peripheral-SpA or reactive arthritis), which leads to a sausage-like appearance
In SpA, low back pain is primarily caused by inflammation of the sacroiliac joints (“sacroiliitis”), which connect the spine to the pelvis. However, sacroiliitis can manifest differently in individuals. Instead of low back pain, some people might report pain in the buttocks, hips, or thighs (6).
Stiffness and pain in SpA can also make movements such as walking or other physical activities difficult. Some people with ax-SpA can even fear moving, which reduces their physical activity (7).
Depending on the SpA type, some people may also experience additional symptoms beyond back and joint pain, including (8):
- Eye pain, redness, and vision changes such as blurry vision or sensitivity to light
- Skin changes, including the appearance of red and silvery-white patches
- Gastrointestinal symptoms such as abdominal pain and diarrhea (which can sometimes be bloody)
Causes and risk factors
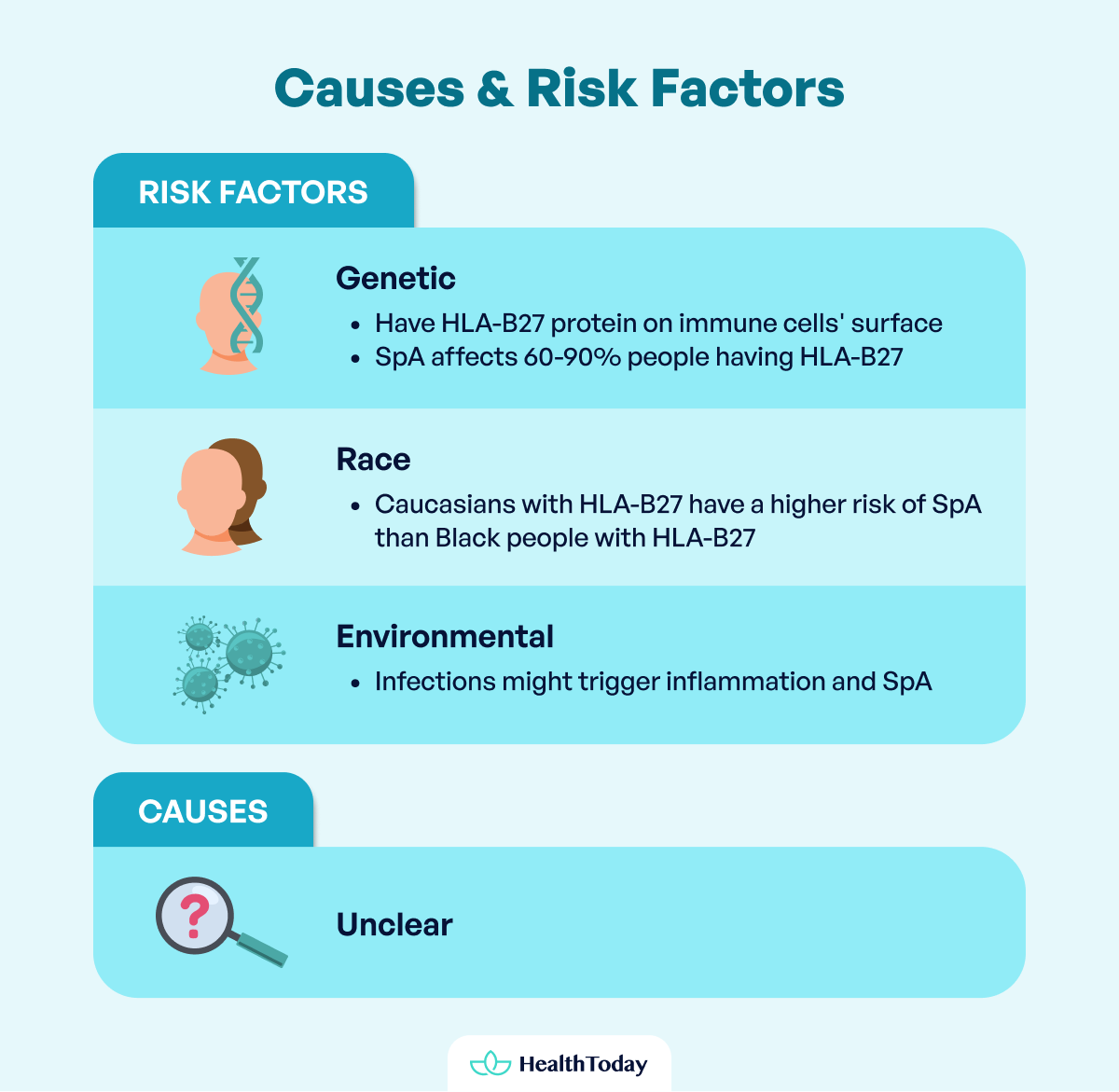
The cause of SpA is still unclear, but experts believe a combination of genetic and environmental factors is involved.
People are more likely to develop SpA if they have a protein called HLA-B27 on the surface of their white blood cells or immune cells. HLA-B27 is a component of a larger protein that helps immune cells recognize and fight foreign invaders such as bacteria and viruses (9).
It is not known exactly how HLA-B27 predisposes someone to develop SpA. However, one hypothesis is that HLA-B27 triggers an autoimmune reaction causing the body’s own cells to attack the spine and joints. Another is that HLA-B27 disrupts the gut microbiome, producing molecules called IL-23 and IL-17 that cause inflammation (10).
Not everyone with HLA-B27 will develop SpA, but most people who have SpA also have HLA-B27. Worldwide, 60 to 90 percent of people with SpA (depending on the type) have HLA-B27 (11). This association is strongest for people with a form of SpA known as ankylosing spondylitis.
HLA-B27, however, does not explain the entire story. In fact, only 1 to 2 percent of people with HLA-B27 develop ankylosing spondylitis (12).
In addition, race may be another factor. White individuals with HLA-B27 are much more likely to develop ankylosing spondylitis compared to Black individuals with HLA-B27 (13). Environmental factors such as infections might trigger immune responses leading to inflammation and the first symptoms of SpA (14).
How can spondyloarthritis cause both bowel issues and hip pain?
In SpA, inflammation can affect the hips and the gastrointestinal tract, causing pain in these areas. A recent study of 165 patients with spondyloarthritis found the following risk factors for hip involvement (15):
- Disease duration over ten years
- Inflammation of the sacroiliac joint, detected based on imaging studies
- Very high disease activity, based on someone’s symptoms and laboratory results
- Functional impairment (difficulty doing specific physical tasks)
- Limited spine mobility
Gastrointestinal symptoms are more common in some types of SpA but can occur in any form of the disease. In a small-scale study involving 65 patients with SpA, 46.2 percent had gut inflammation. This was more common in those who were male, younger, and had severe SpA (16).
People with inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis, may be more likely to develop SpA (17). When SpA occurs in someone with IBD, it’s a type of SpA called “enteropathic arthritis”, where ‘enteropathic’ refers to disease of the intestines.
The link between inflammation involving the intestines and joints is not entirely clear. One hypothesis is that intestinal inflammation makes the gut ‘leaky,’ letting proteins from bacteria and viruses pass through the gut and enter the joint spaces. The immune system then mistakenly attacks the joints while trying to eliminate these proteins, which causes pain (18).
In 2020, IBD affected 2.39 million Americans, mostly starting in young adulthood, which is also when SpA is most commonly diagnosed (19). A study of 350 patients with IBD indicated that over a third had at least one feature of SpA (17). Over a quarter of these patients who saw a rheumatologist were formally diagnosed with ax-SpA, and another 30 percent were diagnosed with peripheral-SpA.
IBD can cause any combination of the following symptoms:
- Abdominal pain
- Diarrhea, which may be associated with blood or mucous
- Losing control of the bowels (fecal incontinence)
- Urge to pass stools without being able to do so
- Constipation
- Nausea and vomiting
- Weight loss
- Fatigue
Abdominal pain in the right and left lower abdomen are more likely to occur in Crohn’s disease and ulcerative colitis, respectively.
Some other types of SpA that can involve both hip and bowel pain include:

- Ankylosing spondylitis: This can cause the bones in the spine to fuse, resulting in reduced spine flexibility and changed posture over time. Some people with ankylosing spondylitis have trouble breathing as their disease progresses to involve the ribs. They often have axial SpA leading to back, hip, buttock, and groin pain, and up to 50 percent of individuals also have IBD (20).
- Psoriatic arthritis: This occurs when the joints become inflamed in people with the skin condition psoriasis. For most people with psoriasis, it takes 7 to 8 years to develop arthritis, if it occurs at all (21). Nail deformities can also occur in this condition. Psoriatic arthritis usually affects joints outside of the spine, but it can rarely cause hip pain. Data from hospitalized patients in the United States from 2000 to 2014 showed that patients with psoriatic arthritis had a significantly increased risk of having IBD compared to patients without psoriatic arthritis (22).
- Reactive arthritis: This is a rare form that occurs days to weeks after an infection of the gastrointestinal or urinary tract. People often begin with bowel symptoms such as pain and diarrhea. After these symptoms resolve, individuals may experience joint pain (typically involving the legs, but sometimes the hips) (23).
Finally, corticosteroid medications, which are often used to treat IBD, may also cause hip pain as anegative effect. People taking high-dose corticosteroids for long periods may experience avascular necrosis, a condition where the bone near the hip is partly destroyed due to loss of blood supply (24). This can lead to pain and decreased mobility and often requires surgical treatment.
Diagnosis
To diagnose SpA, your doctor will take various approaches, including a detailed history, physical examination, laboratory tests, and imaging studies.
If your doctor suspects that you might have SpA based on your symptoms, family history, and examination findings, they may order tests for HLA-B27 and other inflammatory markers in your blood.
They may also take X-rays of your spine and pelvis. If these do not show evidence of inflammation, magnetic resonance imaging (MRI) scans may be required (5). MRIs are especially helpful for ruling out other common causes of hip pain besides SpA.
A person diagnosed with SpA who develops gastrointestinal symptoms such as pain, constipation, or diarrhea must be evaluated for IBD. A gastroenterologist may perform blood tests, stool tests, imaging studies, and ultimately, an endoscopy or colonoscopy to examine the intestines and obtain samples (biopsies) (25).
If tests show that a person with SpA does not have IBD, they may instead be evaluated for irritable bowel syndrome, which occurs more frequently in SpA compared to healthy individuals (4).
Irritable bowel syndrome usually manifests with changes in stool appearance and frequency of bowel movements or pain that worsens or improves with bowel movements. It is diagnosed based on the pattern of symptoms and other tests that rule out other bowel disorders.

Treatment and prevention
Currently, there is no prevention or cure for SpA. However, it is a manageable condition. Treatment aims to relieve symptoms, limit disease progression, and maintain function so that people with SpA can have the best quality of life possible (26).
Medication classes used to treat SpA include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, naproxen, or celecoxib
- Biologics, such as tumor necrosis factor (TNF) inhibitors, interleukin-17 (IL-17) inhibitors, or janus kinase (JAK) inhibitors
Typically, doctors will try NSAIDs first and move on to biologics if NSAIDs don’t work. Corticosteroid injections can also be used to improve inflammation and pain in specific areas. In some cases, surgery may be required to correct severe spine and hip deformities.
People with SpA also benefit from non-medication approaches to treatment, including:
- Education: People should be instructed about the nature of their disease, how to manage symptoms, the importance of medical follow-up, and what to expect with medications.
- Smoking cessation counseling: Cigarette smoking has been associated with worsening spine disease in patients with SpA, particularly among heavy smokers (with more than 10 cigarettes per day) (27).
- Depression screening and treatment: People with SpA have an increased risk of depression compared to patients without SpA. Some estimates show that moderate or severe depression may occur in 15 percent of patients with SpA (28).
- Exercise and physical therapy: Exercise reduces symptoms such as pain, fatigue, and stiffness and improves physical function, heart health, fatigue, sleep, and mood in people with SpA (29, 30). Even people doing well on medications can experience improved symptoms and better spinal movement after participating in rehabilitation exercises (31).
Other causes of right and left hip pain related to bowels
Since SpA is a rare condition, you or doctors might not immediately think of it when hip pain and gastrointestinal tract symptoms occur together. Other conditions can also lead to gastrointestinal pain, which you can sometimes feel in your hips, including:
- Diverticulitis: Diverticulitis occurs when small pouches form in the wall of the colon and become inflamed. Pain typically occurs in the left lower abdomen, while the right side is painful in some people. Other symptoms may include fever, nausea, constipation, or diarrhea (32).
- Colitis: It refers to inflammation of the large intestines. Many symptoms can occur in people with colitis, including watery or bloody diarrhea, abdominal pain, or the urge to pass stools. IBD is one cause of colitis, but many other causes exist, including infections, lack of blood flow, or an adverse effect of medications or radiation therapy (33).
- Appendicitis: This is inflammation of the appendix, a small structure attached to the colon. It usually causes sudden pain in the right lower abdomen. Sometimes, the pain begins around the middle of the stomach and then travels to the right lower abdomen. The pain can worsen with coughing or certain movements. Nausea, vomiting, and loss of appetite can also occur (34).
- Hernia: A hernia occurs when an organ, such as the intestines, pushes through a weak part of the abdomen or groin. In certain cases, a part of the intestines can become stuck, leading to decreased blood flow and severe pain. People can often see or feel a hernia as a bulge in the abdomen or groin (35).
- Gastroenteritis: Gastroenteritis (sometimes called “stomach flu” or “stomach bug”) is inflammation of the stomach and small intestines caused by viruses or bacteria. While you can feel abdominal pain at the sides, it is more common in the middle or lower part of the abdomen. Many people with gastroenteritis also have fever, nausea, vomiting, or diarrhea (36).




Remedies for right and left hip pain related to bowels
If your hip pain results from a gastrointestinal condition, treating the underlying condition is necessary to resolve hip pain. Treatment depends on the underlying cause. Some options include:
- Rest: Some gastrointestinal conditions do not always require medications or surgery. A hernia can be monitored over time if it is not causing problems or worsening. Viral gastroenteritis usually gets better on its own, and staying hydrated helps with recovery.
- Medications: Antibiotics can treat infections in some conditions, such as diverticulitis, colitis, or bacterial gastroenteritis. Anti-inflammatory drugs, corticosteroids, immune system suppressors, and biologics may all play a role in treating IBD.
- Surgery: In some cases, the intestines may be damaged to the point where surgery is necessary. This can occur in severe IBD, diverticulitis, or strangulated hernia.
Depending on the cause, pain medications such as acetaminophen (Tylenol) or NSAIDs may also help relieve pain due to a gastrointestinal condition.
However, they must be used cautiously because pain medications have been shown to increase the risk of some gastrointestinal complications (37). Always consult your doctor before starting any new medications to treat pain related to the bowels.
New findings
Unfortunately, SpA can be very difficult to treat even with the best available therapies. People usually begin treatment with NSAIDs.
If these are not effective, the patients move on to a medication called biologics, which uses the immune system to reduce inflammation and treat disease. However, up to 40 percent of people with SpA fail to respond to biologic therapy (38).
Scientists continue to study new approaches to treat people with SpA. Recently, a class of biologics called IL-17 inhibitors was shown to improve SpA that did not respond to a more popular class of biologics called TNF inhibitors (39). Unfortunately, these medications also worsened IBD, making them a poor option for people who may have gastrointestinal pain from IBD (40).
A newer class of biologics called JAK inhibitors can also be used for people with SpA who fail treatment with TNF inhibitors. However, JAK inhibitors have been shown to carry several risks, including blood clots, cancer, and heart problems (41).
Several recent studies have shown promising results combining medications from different biologic classes to treat patients who have both SpA and IBD (42, 43, 44). However, further research is needed to determine whether these combinations are safe for long-term use.




Can hip pain cause abdominal pain?
While hip pain and abdominal pain might seem unrelated, some people with hip pain might also experience it in their abdomen. That’s because some nerves connect both areas.
A strain in muscles called the hip flexors can cause pain in the front of the hip that travels up to the lower abdomen. Additionally, in some cases, pus-filled collections called abscesses can cause hip and abdominal pain (45). However, it is more common for people with abdominal pain to feel it in their hips (46).
Can appendicitis make your hip hurt?
Yes. This is because the appendix is located in the right lower abdomen, close to the right hip. Some people who have appendicitis will feel pain when they flex their right knee and rotate their hip inward (a positive obturator sign). Others will feel pain when they extend their right hip (a positive psoas sign) (47).
Can irritable bowel syndrome cause hip pain?
People with irritable bowel syndrome (IBS) usually do not have hip pain. However, some people with IBS can describe pain in the lower abdomen that they feel closer to the hips.
Additionally, people with IBS who have constipation may strain regularly to use the bathroom, which can tighten the muscles around the hips and cause pain. However, hip pain is much more likely to result from another condition instead of IBS, including appendicitis, diverticulitis, and colitis.
Can constipation cause hip pain?
Constipation usually does not cause hip pain. Yet, regular straining to use the bathroom can make the muscles surrounding the hip and pelvis tighten, causing pain that is felt closer to the hips.
Can spondyloarthritis-related hip pain lead to mobility issues?
Yes, people with hip pain due to spondyloarthritistypically have difficulty with mobility. Stiffness is a common feature of spondyloarthritis, which can make walking difficult. This can lead to fear of physical activity, which can worsen spondyloarthritis pain since activity is an important part of treatment for this condition (7).
Summary
People with spondyloarthritis can experience hip pain, but this symptom is more common in some types of spondyloarthritis, such as ankylosing spondylitis. Many people with spondyloarthritis also have inflammatory bowel disease or irritable bowel syndrome, which causes abdominal pain that some people feel in the hips.
Treating pain in the hips and bowels in people with spondyloarthritis can be challenging and often requires multiple approaches, including medications and exercise. More research is needed to determine the best and safest way to treat people who do not benefit from existing therapies.

















Comments
0